Resolution of a moderate scoliosis in an infant patient using a ScoliBrace
Summary:
This case demonstrates the successful resolution of a large scoliosis in a female infant using a rigid thoracolumbosacral orthosis. The infant presented with a 44° left, thoracolumbar curve that had been unresponsive to chiropractic treatment. The patient was prescribed a Scolibrace which she wore on a part-time basis for eight months.
The patient was supervised at all times during the wearing of the brace and the brace was only ever worn during the day. A follow-up assessment performed 23 months after the child first presented was unremarkable, with no evidence of scoliosis or postural asymmetry. The bracing regimen was relatively well-tolerated by the patient and her parents.
Case Background
The patient presented to the ScoliCare clinic at 11 weeks of age with a marked ‘C’ shaped scoliosis. The patient’s mother had noticed the curvature in her daughter’s spine soon after birth. The child had been delivered naturally, however the child had “gotten stuck” and support staff had needed to intervene. The child’s shoulder was dislocated at this time, and later relocated.
The mother had taken her daughter to the local chiropractor approximately 1.5 months after the birth for an assessment. The chiropractor had provided a short course of treatment and prescribed gentle bending exercises to help reduce the scoliosis. Unfortunately, the scoliosis had not responded to treatment and was referred to the ScoliCare Clinic.
Examination Findings
The examination performed at the ScoliCare clinic revealed a single, large, left ‘C’ curve (Figures 1A & B). The patient also had difficulty turning their head to the right. The curve was very stiff with little correction during side-bending or traction.
The neurological exam was normal except for a slight reduction in the abdominal reflexes. X-rays ordered soon after confirmed the findings from the physical exam.
The single, left, thoracolumbar curve measured 44° Cobb with an apex at T11. The patient was diagnosed with infantile idiopathic scoliosis and was referred to an orthopaedic surgeon for an evaluation.
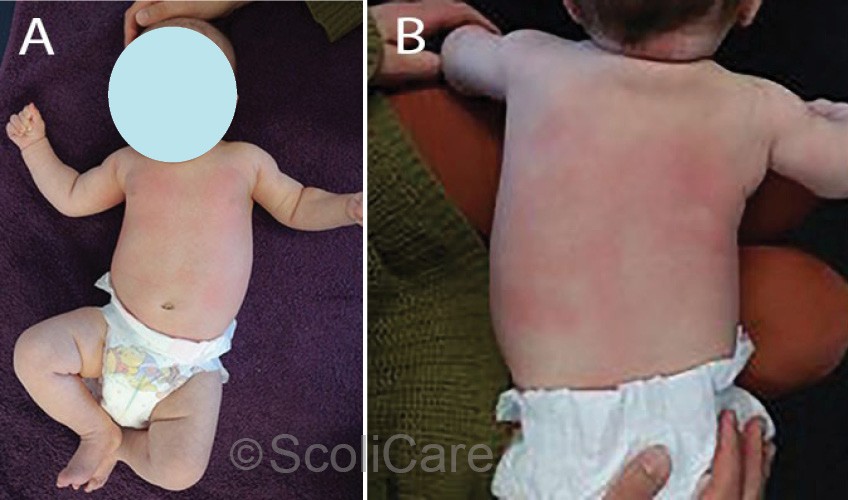
Figure 1: Postural photographs of the infant at the time of the initial consultation.
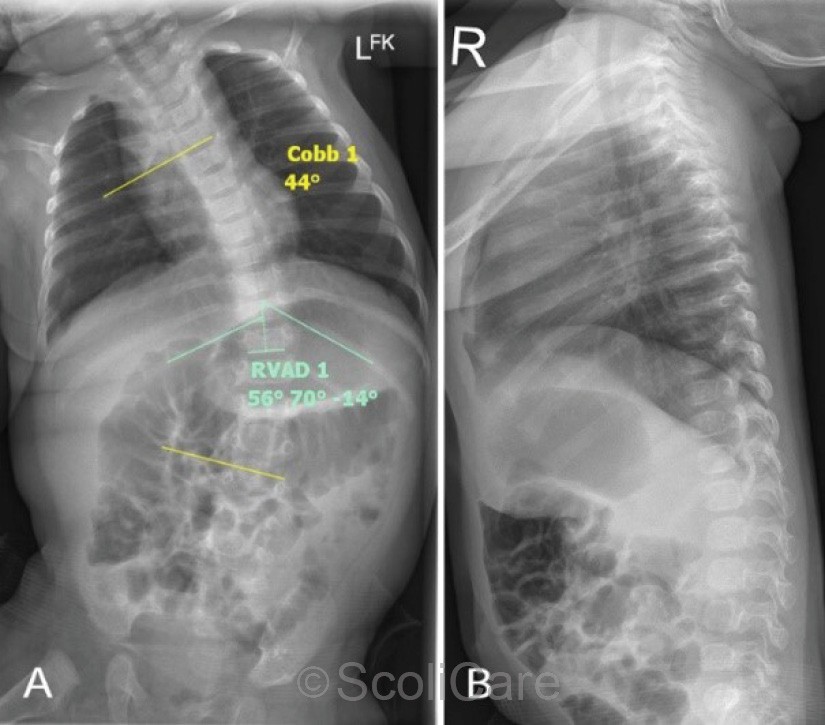
Figure 2: Frontal and lateral x-rays
Intervention
The patient was prescribed a ScoliBrace low-profile, rigid, thoraco-lumbo-sacral orthosis [TLSO] (Figure 3), and scoliosis specific rehabilitation. Part-time brace wear (16 hours per day) was advised and the patient was instructed to use the ScoliRoll traction-fulcrum device (Figure 3) on the primary and secondary curves.
The other component of the rehabilitation program involved Scientific Exercise Approach to Scoliosis (SEAS) rehabilitation exercises performed daily. In addition to the brace and the rehabilitation procedures, the patient was also recommended to wear a shoe lift (20mm) and a heel lift (8mm) to address the leg length discrepancy. The patient was also provided with an ischial lift to use whenever seated to counter the effects of the sacral/pelvic obliquity on the patient’s curves.
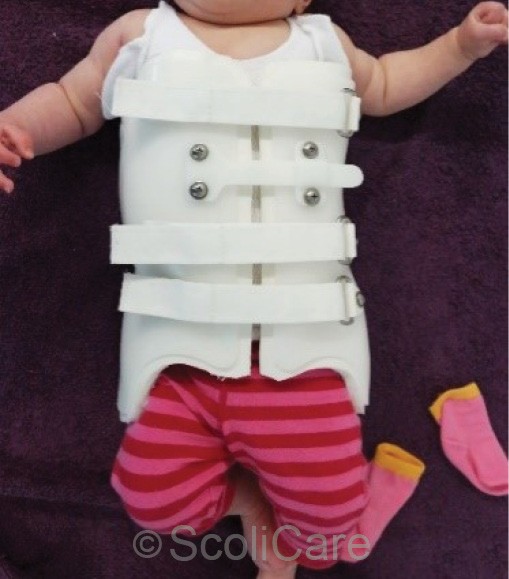
Figure 3: Patient wearing the ScoliBrace orthosis
Outcomes
The patient wore the ScoliBrace on a part-time schedule for eight months. At the end of the bracing period, the child’s scoliosis had been reduced from 44° down to 7° (Figure 4). A follow-up examination was performed 23 months after the initial presentation. The angle of trunk rotation measured 0° at this time and there was no evidence of scoliosis or movement abnormalities.
The parents were very happy with the result and reported that, although challenging at times, the treatment was tolerated by the child.
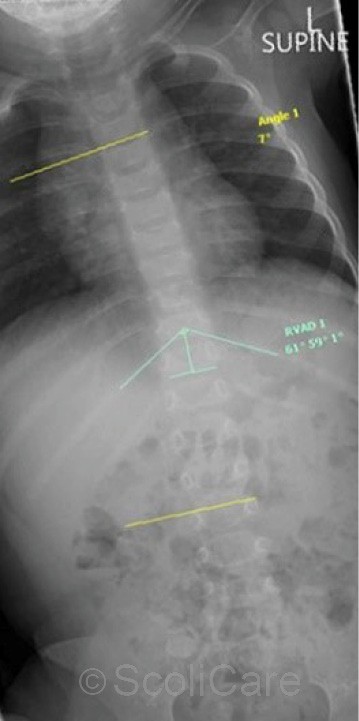
Figure 4: Frontal x-ray taken after the patient had been out of the brace for four months
Discussion
Infantile idiopathic scoliosis presents before the age of 3 years and is classified into two types – resolving and progressive.
Curves in patients with the resolving type tend to reduce spontaneously over time, whereas curves in patients with the progressive type continue to worsen leading to crippling deformity and reduced quality of life if not treated. There are x-ray markers that can be used to differentiate between the two types.
However, the difficult aspect for clinicians dealing with patients with idiopathic infantile scoliosis is that the two types can present identically in the initial stages. Observation is recommended as the initial action, however this can be challenging for parents and clinicians as they wait for a worsening in the patient’s deformity, which, may already be quite significant.
For patients with the progressive type of infantile scoliosis, the standard treatment involves placing the infant in a straightened position then applying a plaster cast. As the child grows, the casts are removed and replaced. This process is repeated, for years in some cases, until the scoliosis has been reduced. The casting process involves intubating and placing the infant under a general anaesthetic.
A surgeon, anaesthetist, nursing staff and a specialist table are required for the procedure, which takes approximately 90 minutes. While casting is successful in the management of most cases of infantile idiopathic scoliosis, there are concerns that the frequent exposure to anaesthetising agents may be damaging to the developing brain of the infant. Treatments such as bracing may represent a safer alternative, but further research is required in this area.
Conclusion
This case study demonstrates the successful management of a moderate infantile idiopathic scoliosis using a ScoliBrace orthosis.
NB: Results vary from case to case. Our commitment is to recommend the most appropriate treatment based on the patients type and severity of scoliosis.

