Postural Improvement and reduced pain in an elderly female patient with adult spinal deformity using a ScoliBrace
Summary:
TThis case highlights improvements in pain, function and postural deformity in a 78-year-old patient using a ScoliBrace orthosis combined with physiotherapeutic scoliosis specific exercises. The patient presented with a 25 degree right-sided lumbar scoliosis and significant coronal imbalance. The patient was prescribed a rigid thoracolumbosacral orthosis to be worn part-time combined with specific daily exercises to help the patient to maintain proper spinal alignment.
The patient was treated for 14 months. The treatment was effective at reducing the patient’s pain and improving their function and quality of life. Significant postural changes were also observed early on in the treatment process and have persisted up to the most recent follow-up appointment.
Case Background
The 78-year-old retiree presented to the ScoliCare clinic with pain, postural problems and spinal deformity. The patient had been diagnosed with scoliosis when she was young but had not received any specific treatment aside from anti-inflammatory medications for the pain associated with her condition. The patient had previously participated in pool-based exercises and pilates, however she had discontinued these activities due to pain.
The patient enjoyed gardening but now found this activity challenging because of her spinal symptoms. The patient was involved with the care of her husband who had suffered a stroke approximately 4 years prior to the consultation at the ScoliCare clinic. She mentioned that playing the role of carer for her husband was stressful and involved frequent bending and lifting.
Examination Findings
The patient stated that her main concerns were that her scoliosis would progress and that the pain that she was experiencing would intensify. She was also aware of the associated postural deformity which impacted negatively on her self-image. The patient completed the Scoliosis Research Society questionnaire (SRS-22r) which revealed very low scores in the function (1.8) and self-image (1.8) domains. The patient reported that she would experience pain most days which was relieved by anti-inflammatory medication and bed rest.
There was a possible family history of scoliosis with the patient stating that her father had suffered from a curvature in his spine. With reference to medical history, the patient had given birth to three children and was currently receiving treatment for a psoriatic skin condition. The patient had suffered a compression fracture of L4 eight years prior to the consultation.
An apparent leg length inequality of 1.5cm was discovered at this time. X-rays taken four years later demonstrated a retrolisthesis at L4/L5. The finding of a compression fracture had prompted a bone mineral density (BMD) evaluation which highlighted that the patient was osteoporotic (Lumbar spine BMD= 0.86 gm/cm2 [T score= -2.6], Right femoral neck BMD= 0.702 gm/cm2 [T score= -2.5]). The patient had been undergoing infusions which was helping to improve BMD for the past four years since her diagnosis.
The physical examination revealed postural abnormalities, specifically right coronal imbalance attributed to pelvic and/or lower limb discrepancy/deformity, bilateral bunions, asymmetrical waist curves and an overt curvature in the lumbar spine (Figure 1).
Lumbar range of motion was reduced in all directions. The angle of trunk rotation was 10° on the right. Nachlas test produced pain in the sacroiliac joint bilaterally. The FABER test provoked hip pain when performed each side. There was pain to palpation over the entire lumbar spine, particularly from L3-S1. The neurological exam was unremarkable.
Plain films demonstrated a mild-moderate right lumbar scoliosis measuring 25° (Cobb) with an apex at L2/3 intervertebral disc (Figure 2). Extensive degenerative change in the lower lumbar spine was noted. The patient was diagnosed with progressive idiopathic scoliosis into adulthood.

Figure 1: Posteroanterior postural photograph (Left), Lateral postural photograph (Right).
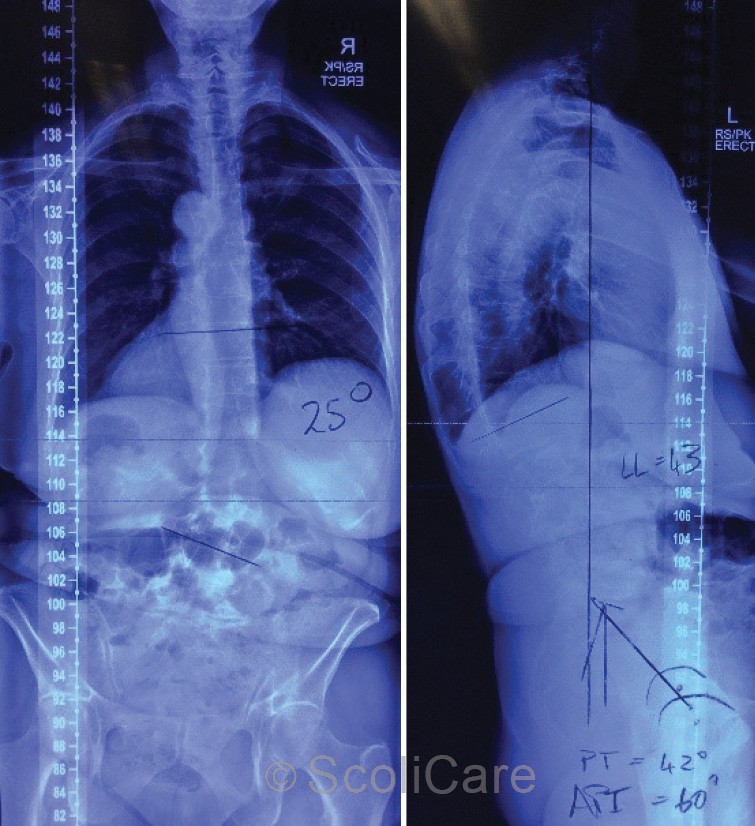
Figure 2: Posteroanterior full-spine x-ray highlighting a 25° (Cobb) right lumbar scoliosis (Left), Lateral full-spine x-ray (Right).
Intervention
The patient was prescribed a rigid thoraco-lumbo-sacral orthosis (TLSO) [ScoliBrace] to be worn on a part-time basis. The patient was also advised to take part in a physiotherapeutic scoliosis specific exercise (PSSE) program.
Due to the patient’s age and the level of degeneration observed in the spine, it was recommended that the patient view the bracing and exercise program as a long-term palliative care strategy. The patient was advised to wear the brace initially for two hours each day then increase the wear by one hour each day up to a level that was tolerable.
The patient was also enrolled in a short program of exercise rehabilitation. The idea of the rehabilitation program was to teach the patient specific exercises to strengthen the muscles around the spine to complement the action of the brace.
Outcomes
The patient was fitted with the TLSO one month after the initial consultation. Postural photographs taken at the time of the brace fitting revealed notable postural improvements in the sagittal and coronal planes (Figure 3).
Plain films demonstrated that there was no significant change in the magnitude of the curve in-brace, however the patient’s coronal balance was significantly improved with the patient’s posture being more aligned with the central sacral vertical line through C7 and S2 (Figure 4).
One month after the brace fitting the patient reported that they had been wearing the brace each day since the fitting. The patient stated that she had experienced some mild constipation in the early stages of brace-wear, but this had passed, and she felt more stable in the brace. She had also noticed that her posture was improved.
The patient was advised to be more active in the brace to build strength and endurance in the muscles that support the spine whilst being held (by the brace) in a more normal postural alignment. This was further reinforced by having the patient perform scoliosis specific exercises at home each day. The focus of these sessions was to teach the patient how to actively place their body in correct spinal alignment through muscular contraction.
In addition to these active self-correction exercises, the patient was also given floor exercises to promote activation of the muscles involved with trunk stabilisation.
The patient is still under care, however at the most recent follow-up appointment (14 months of treatment) the patient stated that she was wearing the brace for 7 hours each day and completing the exercises regularly throughout the week. The patient reported that the brace was helpful most of the time. The exercises did cause cramping on occasion but seemed to be having a positive effect.
Postural photos taken at the most recent follow-up appointment demonstrate a stabilisation of the patient’s postural changes in the coronal and sagittal planes (Figure 5 & 6). The patient’s scores on the SRS-22r have remained relatively stable with clinically significant improvements noted in the ‘function’ domain. The patient has been advised to continue with the part-time bracing and exercise program to maintain the improvements that have been achieved thus far.

Figure 3: Posteroanterior in-brace postural photograph (Left), Lateral in-brace postural photograph (Right)
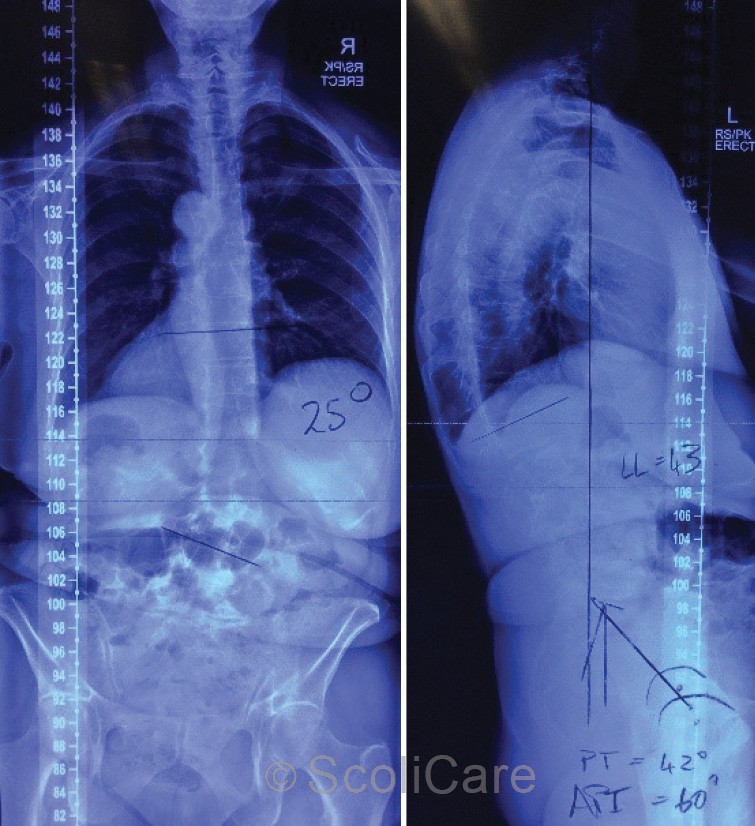
Figure 4: Posteroanterior in-brace x-ray (Left), Lateral in-brace x-ray (Right)

Figure 5: Posteroanterior postural photograph in-brace (Left), Lateral postural photograph in-brace (Right)

Figure 6: Posteroanterior postural photograph out-of-brace (Left), Lateral postural photograph out-of-brace (Right)
Discussion
Scoliosis that is detected in adolescence can progress into adulthood. This progression is most pronounced in patients entering adulthood with scoliosis measuring >30° (Cobb).
It is well known that postural changes associated with scoliosis, specifically coronal and sagittal imbalance, can lead to pain and reduced quality of life in patients as they age. Furthermore, any departure from normal alignment tends to compound the effects of the natural degenerative process that occurs with aging. Coupled with decreases in skeletal muscle mass (sarcopenia) and bone mineral density (osteoporosis) that occur over time, adults with spinal deformity can suffer immensely as they age.
In adolescent patients, conservative management strategies such as bracing and exercise have demonstrated efficacy in stabilising or even reducing scoliotic curves. Unfortunately, using conservative treatments to mould and shape the spine is far less effective when applied to a skeletally mature patient.
For this reason, care of adult patients with scoliosis should be viewed as being more palliative/preventative than corrective. Bracing in adults, as demonstrated by this case, can be used to move a patient closer to a more ideal spinal alignment. Exercises can be used to maintain muscle mass and strengthen muscles involved with trunk stabilisation.
The results of conservative management in adult scoliosis patients are certainly less spectacular in terms of measurable changes in Cobb angle, however these types of therapies do create clinically meaningful changes to a patient’s pain, function and quality of life.
Conclusion
SThis case demonstrates the successful management of an elderly female patient with progressive idiopathic scoliosis into adulthood using a ScoliBrace and scoliosis specific exercises. While significant curve reduction is not realistic in this age group, this case demonstrates that meaningful postural correction and improvements in pain, function and quality of life can be achieved with a conservative approach.
NB: Results vary from case to case. Our commitment is to recommend the most appropriate treatment based on the patients type and severity of scoliosis.

