Correction of a 33° thoracolumbar Scoliosis using a ScoliBrace orthosis and Scoliosis Specific Rehabilitation
Summary:
This case details the correction of moderate thoracolumbar scoliosis in a 13-year-old female patient using a ScoliBrace orthosis combined with scoliosis specific rehabilitation. The patient presented with a 33° thoracolumbar scoliosis (Risser 1-2), pain that was interfering with her quality of life, and altered self-image.
The patient was prescribed a rigid ScoliBrace to be worn full-time and advised to perform SEAS exercises and use the ScoliRoll orthosis daily. The patient wore the brace full-time for 17 months then on a part-time basis for a further 17 months. At the end of the treatment regimens, the patient’s curve had been reduced to 10° and there was a significant improvement in the aesthetic appearance of the trunk.
Case Background
The patient presented to the ScoliCare clinic at age 13 with a recent diagnosis of adolescent idiopathic scoliosis (AIS). The patient was experiencing mild back pain and had noticed that her posture was asymmetrical.
The patient was involved with sport (ballet, dance and netball) four days per week on average.
Examination Findings
There was no family history of diagnosed scoliosis. The patient had begun her menses in the year proceeding her visit to the clinic.
The total score for the Scoliosis Research Society questionnaire (SRS-22r) was 3.18 with the lowest scores seen in the pain (2.8) and self-image (2.8) domains. On physical examination, an obvious spinal curvature with left coronal imbalance (Figure 1) was noted.
The Adam’s forward bend test was positive, with an associated angle of trunk rotation measuring 12° in the thoracolumbar region. Initial x-rays showed a 33° left thoracolumbar scoliosis (Figure 1). The patient was Risser 1-2.
Given the skeletal immaturity of the patient and the magnitude of initial scoliosis, there was a high risk of progression in this case.
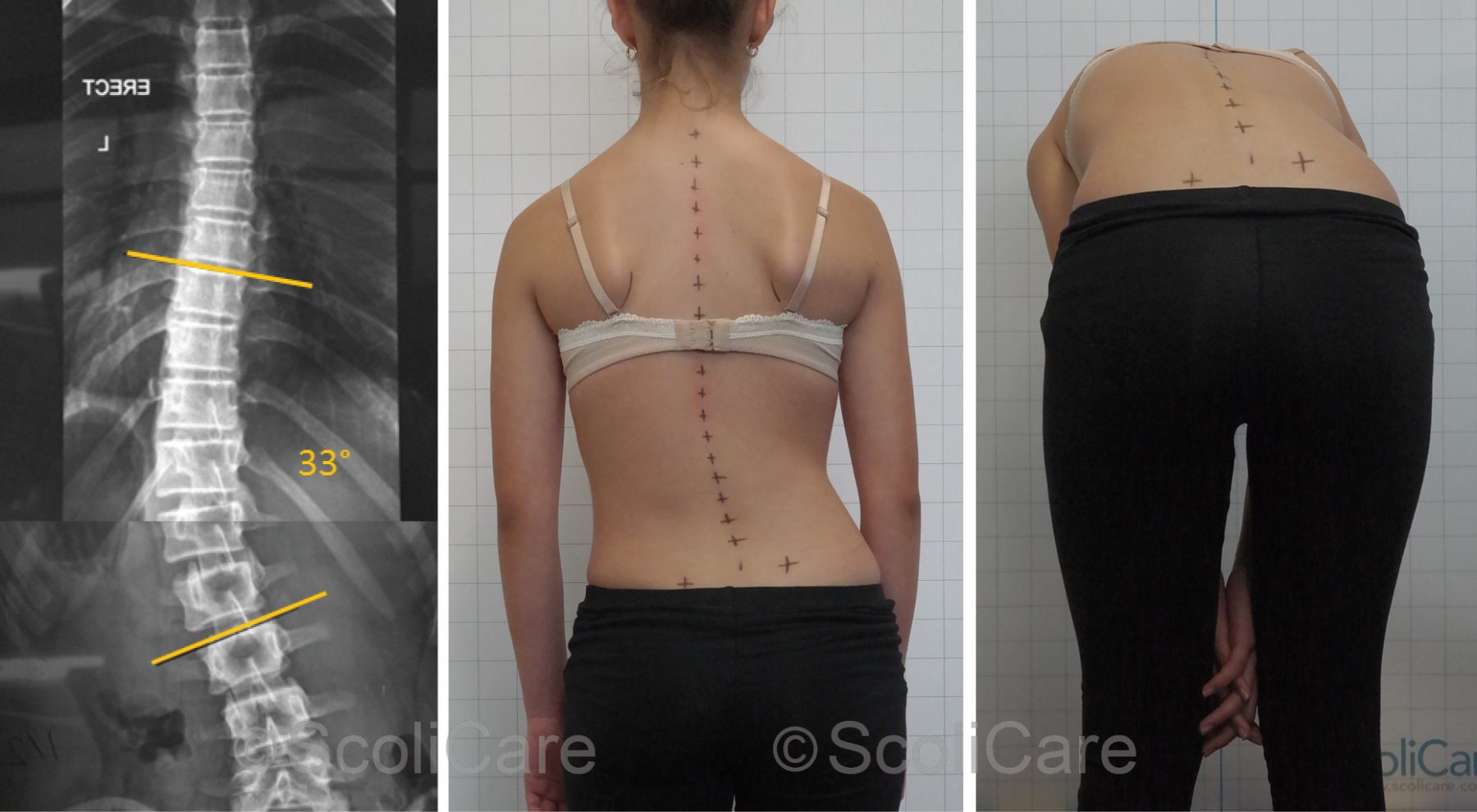
Figure 1: Posteroanterior thoracolumbar x-ray (Left), Posteroanterior postural photograph (Middle), Adam’s forward bend test photograph (Right).
Intervention
The patient was subsequently prescribed a customized, three-dimensional, rigid, thoracolumbosacral orthosis [TSLO] (ScoliBrace) [Figure 2] and scoliosis specific rehabilitation. Full-time (23 hours per day) brace wear was recommended, however, the patient was informed that they could wear the brace for as little as 20 hours per day provided they were participating in ballet, dance or netball on that day.
With regards to the rehabilitation component of the patient’s treatment program, the patient used the ScoliRoll orthotic device and performed exercises based on the Scientific Exercises Approach to Scoliosis (SEAS) principles.
The ScoliRoll was also incorporated in the rehabilitation program and the patient was instructed to lie on the device daily for up to 20 minutes, with the peak of the device positioned at the apex of the thoracolumbar curvature (Figure 2). The concept behind this placement is to encourage movement at and around the apex of the patient’s primary curve. The patient also performed basic exercises on the ScoliRoll.
The SEAS exercises were performed under guidance in the clinic twice per week for 3 weeks, then once per month after that point. The patient was also instructed to perform the rehabilitation exercises and use the ScoliRoll daily. The exercises were progressed, with more difficult variations added, as the patient made improvements in strength and endurance.

Figure 2: Posteroanterior photograph of the patient wearing the ScoliBrace (Left), Photograph of the patient side-lying on the ScoliRoll orthosis (Right).
Outcomes
In-brace plain films taken 1 month after the brace fitting demonstrated a significant reduction of the patient’s scoliosis – from 33° down to 13° (Figure 3).
Out-of-brace x-rays taken 3 months after the brace fitting showed a reduction of the scoliosis down to 26° (Figure 4). The patient continued full-time bracing for 17 months.
The brace was then worn only at night for another 17 months. The most recent x-rays demonstrate that the patient is Risser 4 and the scoliosis has been reduced by 23° over the course of the treatment (Figure 5).
The patient’s posture improved continuously during the treatment program, with minimal asymmetry observed at the most recent follow-up consultation (Figure 5).
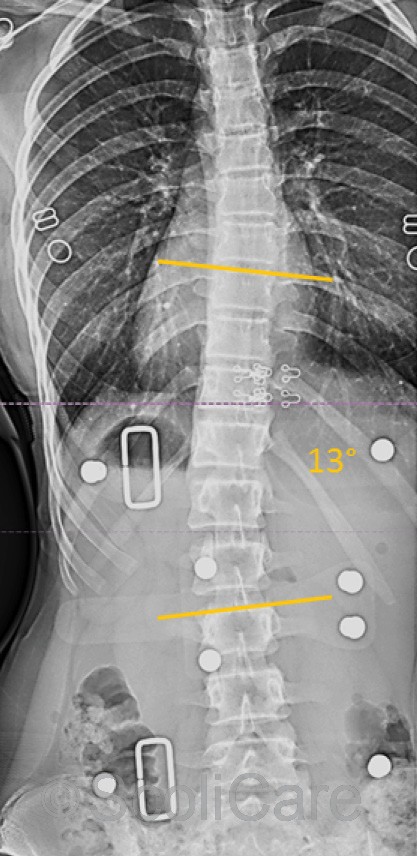
Figure 3: Posteroanterior 1-month, in-brace x-ray (13° Cobb)
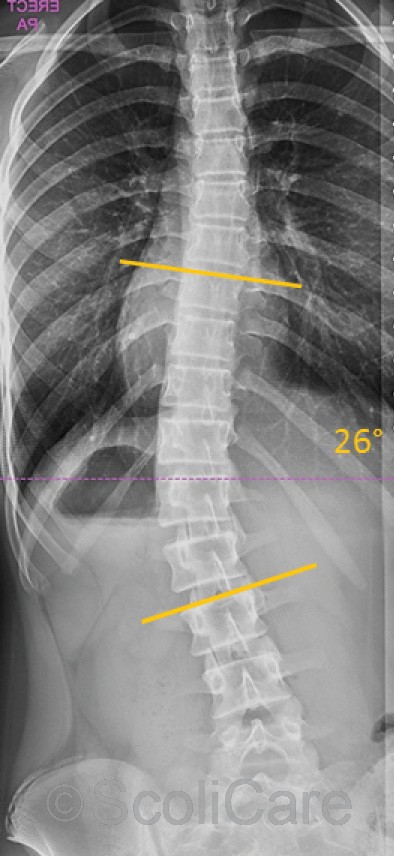
Figure 4: Posteroanterior 3-month, out-of-brace x-ray (26° Cobb)
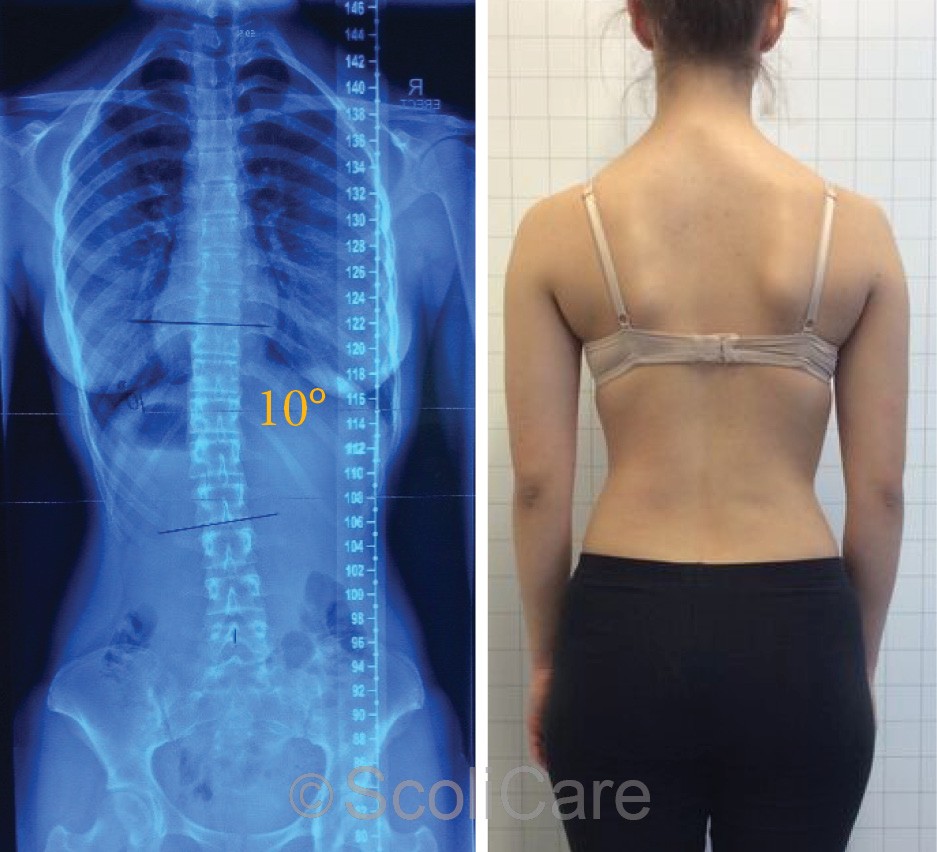
Figure 5: Posteroanterior out-of-brace x-rays (32 months) [10° Cobb] (Right), Posteroanterior postural photograph (Left)
Discussion
Large scoliotic curves give rise to surface deformities such as rib humping and postural asymmetry. These physical changes can negatively impact on the quality of life of AIS patients. This was evident in this case with the patient reporting pain and altered self-image on the initial consultation. Moreover, curves measuring above 30° often contribute to pain, disability, functional limitation, reduced quality of life and pulmonary problems in adulthood.
For this reason, it is important to implement treatment strategies to stabilize and/or attempt to reduce clinically relevant curves as soon as they present in AIS patients.
Bracing is typically used to halt the progression of scoliosis in AIS patients with curves measuring >20°. For some patients, as highlighted by this case, bracing can be used to reduce abnormal curvatures and restore normal postural alignment. It is also common practice to combine physiotherapeutic scoliosis specific exercises and various forms of active and passive mobilization techniques as adjuncts to the bracing therapy.
Conclusion
This case demonstrates the reduction of a 33° thoracolumbar scoliosis using a custom designed three-dimensional scoliosis brace, in combination with a scoliosis specific rehabilitation program. This approach may be of benefit to AIS patients with moderate sized thoracolumbar curves.
NB: Results vary from case to case. Our commitment is to recommend the most appropriate treatment based on the patients type and severity of scoliosis.

